The term “root canal” refers to both a dental procedure and a part of the tooth. It involves the removal of infected or damaged tissue within the tooth’s canal, aiming to save a tooth from extraction. This treatment addresses severe tooth decay or infection, alleviating pain and restoring oral health. Understanding the meaning of root canal is crucial for individuals seeking relief from tooth-related discomfort and preserving their natural teeth.
What is a root canal?
The procedure known as a root canal involves the extraction of the tooth’s pulp, which consists of nerves, connective tissue, and blood vessels. Typically, a general dentist or endodontist will administer local anesthesia before performing this procedure. Find out more about this commonly performed treatment and the possible risks associated with it.
When is a root canal needed?
When the soft inner part of a tooth, known as the pulp, becomes inflamed, injured, or infected, a root canal is necessary. Although the crown of the tooth may remain intact, removing the damaged pulp is the best way to preserve the tooth’s structure.
The pulp can become damaged due to untreated cavities, multiple dental procedures on the same tooth, a chip or crack in the tooth, or an injury to the tooth.
Common symptoms of damaged pulp include pain in the tooth, swelling, and a sensation of heat in the gums. To confirm the diagnosis, the dentist will examine the painful tooth and take X-rays. If a root canal is needed, the dentist may refer the patient to an endodontist.
See more: Exploring the Causes and Treatment of Dental Pulpitis
How is a root canal performed?
In a dental office, a root canal procedure is carried out. Upon your arrival for the appointment, a technician will accompany you to a treatment room, assist you in getting settled in a chair, and place a bib around your neck to shield your clothes from stains.
Step 1: Anesthetic Application
The dentist administers numbing medication on the gum adjacent to the affected tooth. Following this, a local anesthetic is injected into the gums. While you may experience a brief sharp sensation or slight burning initially, this discomfort swiftly dissipates. Throughout the procedure, you will remain conscious, yet the anesthetic ensures you won’t feel any pain.
Step 2: Pulp Removal
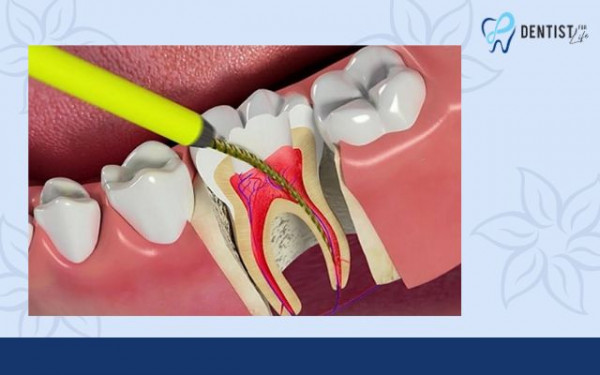
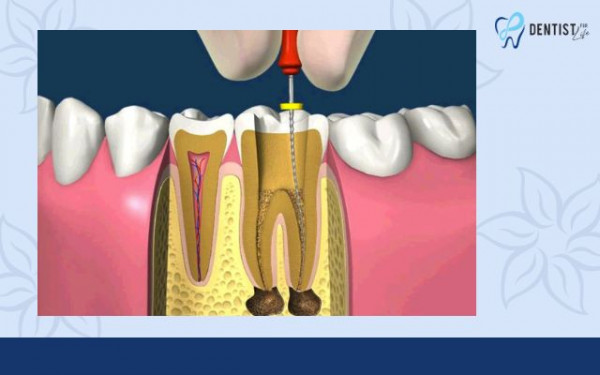
Once the tooth is numb, the endodontist or general dentist creates a small opening at the top of the tooth. With specialized instruments called files, the infected or damaged pulp is meticulously removed. Thorough cleaning of the tooth’s canals is undertaken to ensure complete removal of the affected tissue.
See more: What is periodontics? What is periodontitis? Cause and signs of identification
Step 3: Antibiotic Application
After the pulp extraction, a topical antibiotic may be applied to the area to eradicate any remaining infection and prevent reoccurrence. Subsequently, the cleaned and disinfected canals are sealed with gutta-percha, a rubber-like material, and a sealing paste. Additionally, oral antibiotics may be prescribed for further infection control.
Step 4: Temporary Filling
To conclude the procedure, a soft temporary filling material is used to seal the small opening at the tooth’s top. This temporary sealant serves to safeguard the canals from potential damage caused by saliva.
What are the indicators of a root canal infection?
Signs and symptoms of a root canal infection may include:
- Persistent, severe tooth pain unrelieved by pain medication
- Intense toothache when biting or chewing
- Swollen and tender gums
- Presence of pus around an infected tooth
- Sensitivity to hot or cold that lingers after the hot or cold stimulus is removed
- Loosening of a tooth
- Swelling of the face or neck
Darkening of the affected tooth It is also possible to have deep tooth decay without experiencing any pain or discomfort. The decay or infection may be discovered during an x-ray examination performed by a dentist or endodontist.
When to Consult Your Dentist or Endodontist:
Seek urgent dental attention if you experience intense pain or swelling. Your dentist might refer you to an endodontist for specialized care if necessary.
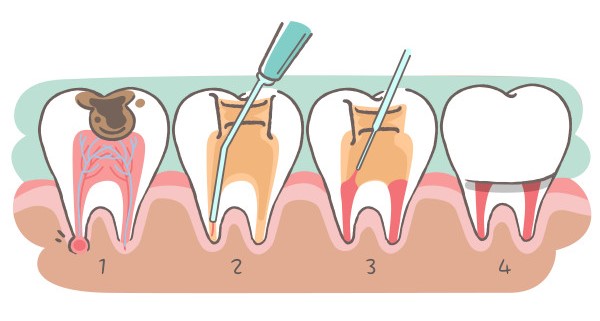
Root Canal Treatment Procedure Overview:
- Root canal treatment usually spans multiple appointments. Here’s what your dentist or endodontist will do:
- Take an X-ray of the tooth and surrounding area.
- Apply local anesthesia to numb the tooth area.
- Place a rubber dam over the tooth for cleanliness.
- Drill a hole in the tooth’s top to access and remove the pulp.
- Thoroughly clean and disinfect the tooth’s canals.
- Apply a temporary filling if multiple sessions are required.
Following the cleaning sessions, fill the canal space with gutta-percha, a sterile material.
Subsequently, your dentist will affix a filling or crown to seal the tooth, preventing further bacterial infection.
See more: Discover Convenient Restorative Dentistry Near Me
Conclusion
At Dentist For Life, understanding the significance of a root canal extends beyond mere definition—it’s about offering patients comprehensive care and relief from dental discomfort. Our commitment to educating and guiding individuals through the intricacies of root canal treatments is coupled with a dedication to providing personalized, precise, and compassionate care.
Root canal procedures aim not only to alleviate pain but also to preserve natural teeth and promote enduring oral health. Trust Dentist For Life for expert guidance and tailored treatments that prioritize your comfort and well-being, ensuring a journey towards a healthier, pain-free smile. Schedule a consultation today and experience our commitment to exceptional dental care.